Feet First: Six Tips To Maintain Healthy Feet and the Freedom To Move
Your feet are among your most important body parts. They get you where you want to go, help you stay healthy through physical activity, and provide freedom of movement. However, it’s easy to take your feet for granted — until you have an injury or problem.
Foot health is important for everyone. Most of us don’t think a lot about foot care, but it’s essential to prevent foot health issues to keep your whole body healthy. Foot health is even more vital for people with diabetes.
The following six tips can help you improve or maintain your foot health and the freedom to move.
1. Clean Your Feet Daily and Wear Clean, Dry Socks
Wash your feet daily in lukewarm water. Avoid using hot or cold water. Water that is too hot or too cold can damage your skin, especially in people with diabetes who have decreased skin sensation. Use a soft washcloth or sponge and gentle soap. Then, rinse thoroughly and dry your feet completely before donning socks and shoes.
When our feet sweat, moisture gets held against our skin by most socks. Socks that are bunched up or too tight around the ankles or calf also can cause irritation or problems. The American College of Foot and Ankle Surgeons warns that having diabetes increases the risk of developing a wide range of foot problems. People with diabetes should consider special socks designed with extra cushioning and moisture-wicking fiber.
2. Inspect Your Feet Regularly
Check your feet for blisters, redness, small cuts, or cracked skin. If you can’t see the bottom of your feet, use a hand mirror with magnification. If you notice any problems, contact a doctor or physical therapist. Never ignore a problem with your feet. If you have diabetes, check your feet daily.
3. Cut Nails Carefully and Regularly
Keep your nails trimmed, but not too short. Nails that are cut too short can become ingrown and cause soreness or infection. It is best to cut nails straight across and then carefully file the edges. If you cannot cut your own nails, a podiatrist can assist. If you use a nail salon, make sure to tell them to be careful not to cut your toenails too short or injure your skin during filing.
4. Always Wear Well-Fitted Shoes
Shoes that don’t fit well may cause blisters that can lead to infection or other problems. Make sure you choose shoes that do not irritate your feet. Wear shoes that properly support your feet and ankles to ensure safety while walking.
A physical therapist can help ensure that your shoes fit properly for general wear or sports-specific activities and recommend shoes or shoe inserts (orthotics) for proper support.
5. Moisturize Your Feet at Night
Keep your skin soft and healthy by moisturizing every night. This can help prevent itching or cracking. Avoid putting lotion between your toes.
6. Keep your Blood Sugar Under Control
According to the National Institutes of Health, diabetes can affect your feet. High blood sugar levels can cause nerve damage, resulting in loss of skin sensation. Reduced blood flow also can make it harder for your feet to heal from an injury or resist infection.
Regular physical activity and proper nutrition are keys to preventing type 2 diabetes and maintaining appropriate blood sugar levels. Whether you have diabetes or not, it is important to get the recommended amount of daily physical activity to prevent and manage many chronic conditions and diseases.
Our physical therapists are movement experts who help people with foot problems improve their quality of life through hands-on care, patient education, and prescribed movement. They also can help people with diabetes improve their strength, balance, and endurance, and maintain good skin health.
H2O: Water Therapy from the Inside Out
Ahhh-swimming; that oh-so-wonderful feeling of being able to cool off on a hot day! Gliding through the water, that is 800 times denser compared to air, de-weighting us to the point where we can, somewhat, believe it brings out the child in us. And why shouldn’t it!? For most of us, we couldn’t wait to run and jump in and splash, and free-stroke.
Yes! Free-stroke equaled Free-dom!
Confidently we become buoyant, meeting a greater resistance by moving our arms and legs through the water (vs. air); hence we feel the restorative powers- like a superhero! And, when we are finished with our swim, whether it was for an hour, or several, we get exercise; pain-Free at that…might even have a little appetite too from so much exertion! Not-to-mention looking a little more toned and sculpted.
With our busy lifestyles, and as we age, we are gonna have aches and pains-and maybe a little joint cracking here and there. You may even be experiencing a little (or a lot) of arthritis now. What to do? Ah-yes, go swimming! Because to be pain-free means you have to move consistently, and frequent movement is a hard sell to those of you in pain! Whether you have musculoskeletal disorders, chronic back pain, need lumbar stabilization (pregnancy), have foot, ankle, knee, or shoulder pain, or any kind of arthritis–results from swimming and aquatic therapy are immediate!
So, rekindle your memory of youth and rebuild your confidence of daily living; pain-Free. Go get in a pool and MOVE; swimming (aquatic therapy)-it’s a high-intensity exercise…….Free yourself today!
Why Physical Therapy is About More Than ‘Getting Better’
When a patient makes an appointment with a physical therapist to rehabilitate after a shoulder injury, for example, it’s because he wants to get better, right? Well, yes, but what exactly does that mean? As it turns out, “getting better” means different things to different patients. To some, proper recovery from a shoulder injury means being able to carry a golf bag and swing a club while to others, it means being able to lift their children in and out of their car seats.
Here’s the thing: Helping your physical therapist know and understand your own personal goals is the key to success. As a patient, that means speaking up early and often about how the injury is limiting the everyday activities that are most important to you. With this knowledge, your PT can adapt her approach and individualize aspects of the treatment plan to ensure that you meet your goals.
It’s part of a physical therapist’s job description to work with patients to reduce pain and to improve strength, range of motion, balance, and mobility. Your PT will address these aspects of your treatment regardless, but if you return home to unload the dishwasher and realize that you still can’t reach to place the coffee mugs on the shelf, then that’s a problem.
Your PT can’t possibly know everything that’s important to you—or the obstacles that you face—unless you share that information with them. One way around this is to bring a list to your first therapy session of the chores that are most important to you in and around your home and the activities that you participate in that bring you the most joy. To take it a step farther, whittling that list down to one main goal can give you something to focus on in therapy—and motivate you to keep showing up and following the home exercise program that your PT designed. That number-one goal may be different for each patient but the desire to attain it should be the same.
With a little effort on both sides, patients and their PTs can work together to individualize the therapy sessions and select the most appropriate interventions. After all, physical therapists want nothing more than to help their patients return to previous levels of function as quickly and effectively as possible.
What’s a Movement Diagnosis?
Medical diagnoses don’t need much of an introduction. They’re what you get from your doctor when you’re sick. Examples would be influenza, diabetes, or hypertension. They describe the underlying problem that is causing your symptoms.
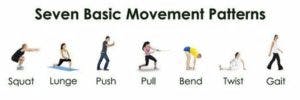
When people feel sick, they know they need to go to the doctor and find out what’s going on to get treated. We should treat movement the same way. If you’re having pain when you move, can’t do things you used to be able to – like get on and off the floor easily, or can’t do things you want to do – like go for a bike ride or pick up a grandchild then you need to get a movement diagnosis.
A movement diagnosis does the same thing as a medical diagnosis; it describes what’s causing your difficulty with movement. Some examples would be difficulty standing from a chair secondary to decreased force production, scapular down rotation syndrome, or lower crossed syndrome.
Diagnoses set the roadmap for treatment, so getting them right is crucial. Human movement is complex and is influenced by more than just your muscles and joints. According to the APTA, movement is impacted by the following systems:
– Endocrine
– Nervous
– Cardiovascular
– Pulmonary
– Integumentary
– Musculoskeletal
Because of the complexity and interplay between these components of the movement system, getting a movement diagnosis correct is often very difficult. Physical therapists are experts in human movement with doctoral-level training and should be your first stop for movement issues.
Not only can our physical therapist provide an accurate movement diagnosis they will also design a treatment plan to correct the underlying issues and help get you moving well again.
References:
https://journals.lww.com/jnpt/FullText/2018/04000/White_Paper__Movement_System_Diagnoses_in.9.aspx
Fitness, with a Side of Dysfunction?
This time of year, many people are focused on fitness so it’s worth taking a look at what fitness really means. The dictionary defines fit as “sound physically and mentally, healthy.” Using that definition, many “fitness” routines fall short of the goal. If you don’t enjoy running and dread every workout, you’re probably falling short of the “sound mentally” portion. Exercise should be enjoyable, reduce stress, and leave you feeling better, not worse.
NO PAIN NO GAIN?
Exercise should also leave you feeling better physically. If you can run a good time in a 5k, but have aches and pains for days after, you’re not “sound physically.” If you are increasing your PR in the squat rack, but your joint pain is increasing right along with it, you’re not “sound physically” either. Sure, some muscle soreness and fatigue after a hard workout is normal. But if you’re having pain that doesn’t go away, sore joints, or trouble moving after exercise, you’re probably developing movement dysfunction along with your fitness.
MOVEMENT DYSFUNCTION
Go back to the dictionary and you’ll find that dysfunction is “impaired or abnormal functioning.” So movement dysfunction is impaired or abnormal movement. When someone has a movement problem like a sore joint, limited range of motion, or strength loss, the brain finds a way to get the body to do what it wants. That usually means moving in a way that is less than optimal. For a while, it works. But eventually, it leads to injury. As a concrete example, think of someone who has trouble bending one knee doing squats. When one knee bends further than the other, it will cause one side of the pelvis to drop lower than the other. Now that the pelvis isn’t level, the spine bends towards the high side to stay balanced. When that one side of the pelvis drops lower than the other one, it also usually rotates. Now the spine has to bend to the side and twist to keep you upright. This works for a while, but as weight gets added to the squat, and the repetitions add up so does the risk for a back injury.
PREVENTATIVE MEDICINE
Pain during workouts, or pain and soreness that don’t go away after can be warning signs of a movement dysfunction. If you’re experiencing any of these, your physical therapist is a movement expert who can help. PTs are trained to analyze movement, and figure out the root cause of problems. They can then design a program to treat the cause and correct the abnormal pattern. There is no need to wait until you’re injured to see your physical therapist. In fact, it’s preferable not to. Getting minor problems fixed early means fewer visits to the PT, less pain, and not having your workouts put on hold by injury.
Physical Therapy Isn’t Just for Pain. It Can Keep You Healthy for Life.
You know that physical activity is good for you. The benefits are well researched and the list is impressive. Here’s just a sampling:
– Releases endorphins to make you feel good and fight depression
– Helps control weight
– Prevents diseases like stroke, diabetes, and some forms of cancer
– Improves sleep
– Helps you live longer
Recent studies even show that physical activity strengthens your immune system, with a protective effect against COVID, and that staying active through middle age protects your brain as you age.
Physical activity is a wonder drug. If it was a pill, you’d buy it and take it every day. But even though activity is free, less than 25% of Americans meet the CDC recommendations for activity. We clearly need help.
Physical Therapists Are The Experts in Human Movement
To be active, you need to be able to move. Physical Therapists do more than help you recover from surgeries or major injuries. They are the experts in human movement. Sure, you could see a strength coach to lift weights, hire a personal trainer, go to a yoga class to work on your flexibility and balance, and see a chiropractor for adjustments. But that seems like a lot of people when a PT can help you with all of these things and more. Nobody knows more about human movement or looks at your health the same way a PT does. Your PT can help you with every aspect of movement including strength, range of motion, flexibility, endurance, balance, and coordination.
As medical professionals, they can help you with injuries or other issues. Your PT can work with your doctor to help use activity to manage things like diabetes, cholesterol levels, or blood pressure instead of prescriptions. Your PT is also trained to work with people of all ages, so you can develop a long-term relationship and they can continue to adjust and modify your routine as you age or your goals change.
Stay Healthy For Life
Staying active has a long list of benefits both now and in the future. But chances are you’re not moving enough to make the most of those benefits. Most people need help. Physical therapists are the most qualified professional in existence to help keep you healthy now and in the future. So don’t think of your PT as someone you see when you need help with pain or an injury. Think of them as your partner and coach working to help you stay healthy for life.
Pelvic Floor PT: When to Go & What to Expect
Pelvic Physical Therapy covers a variety of dysfunctions from pain to incontinence. It has many possible causes and affects up to 20% of the population in the United States, including women and men.
Pelvic pain is quite often overlooked; 61% of women never have a diagnosis. 1 in 7 American women ages 15-80 experience some sort of pelvic pain and physical therapy can help.
Katie Reynolds and Kennan Wyne have specialized training in internal and external examinations of the pelvic floor muscles to determine the tone and strength of the muscles and malalignments of the pelvic girdle.
Physical therapy can help retrain these muscles through Kegel exercises and by keeping a bladder diary. Additional prescribed exercises will help improve/maintain bladder and bowel control, heighten sexual response, maintain strength, tone, and elasticity to support your organs against gravity.
With the help of our specialists, our patients will need a minimum of three to six visits. Usually, after therapy, you are able to sit pain-free, have intercourse without feeling pain, as well as regaining control of your bladder and bowel functions.
Be the Boss of Your Bladder and Bowel!
Urinary Incontinence (UI) is the weakening of the pelvic floor muscles due to trauma/injury, pain, or malalignment of the pelvic bones.
Physical Therapy can help decrease the frequency of having to go and accidental leakage. With the help of biofeedback, modalities (moist heat), and manual therapy (hands-on approaches), most patients will see results in as little as four to eight visits. Urinary Incontinence types are defined as:
Urge: This is when urine loss may occur after a strong and sudden desire to urinate. This happens with only a few seconds or minutes of warning causing the bladder to contract when it is not time.
Stress: This is when a small amount of urine loss occurs with physical exertion. This could be with a cough, sneeze, lift or laugh.
In the past, everyone thought that Kegel exercises were the cure for UI and when leaking continued to occur, frustration forms into a “no hope” attitude. Katie and Kennan treat their patients beyond Kegels. As important as these exercises are it is more important when to perform Kegels in conjunction with exercises for maximum benefit.
Fecal Incontinence (FI) is the recurrent uncontrolled passage of fecal material and certainly can have its detrimental impact on lifestyle and functioning compared to urinary incontinence. FI is also attributed to conditions associated with pelvic floor weakness.
Constipation Blues?

Constipation can affect many individuals and cause increased pain in the abdomen as well as acid reflux. Physical therapy can be beneficial in helping you have a good bowel movement and decrease discomfort. Through education in how the bowels function and abdominal massage, along with other techniques, we can help you with this unpleasant experience.
What to Expect.
Katie or Kennan will create an individualized program that will help them identify what factors aggravate your symptoms based on your diagnosis.
They will incorporate the essential components mentioned previously by closely monitoring diet and fluid intake, bladder irritability, activities of daily living, stressors, and musculoskeletal components.
For patients that have difficulty identifying and isolating the muscles of the pelvic floor, the use of our Biofeedback machine can be used to pick up small electrical stimuli in the muscles and translate these signals into a visual bar graph. As the contraction increases, the visual bar graph gives our patients “feedback” contraction strength and if performed correctly.

Each of our patients are then instructed in a home exercise program designed specifically for their condition, giving them the power and knowledge to regain their quality of life!
5 Reasons You Need a PT to Coordinate Your Fitness Regimen
Physical therapists aren’t just for people that are injured or have had surgery. Physical therapists can also help healthy people improve their fitness. Here are 5 reasons why you should consider seeing yours.
YOU WANT A BASELINE
When you see a physical therapist to improve your fitness, you’ll get an assessment of your strength, range of motion, posture and movement patterns. This not only helps your physical therapist design a customized program just for you, it gives them a baseline to compare things to in the future should you start having pain or suffer an injury.
YOU WANT EXPERT GUIDANCE
Sure, other professionals could help with your fitness routine, but the fitness industry is not well regulated. Some certifications just require an online course and paying a fee. There are no licenses or other requirements to use many titles. Becoming a physical therapist requires at least a bachelor’s degree and most PTs practicing today have a doctorate. Every PT has passed a national board exam and maintains a state license. That guarantees you that every physical therapist is a verified expert in human movement.
YOU WANT TO PREVENT INJURY
Physical therapists don’t just work to heal injuries, they are also experts in preventing them. After a thorough assessment, a PT can help you design a program that will not only help you reach your fitness goals, but that can address any issues that increase your risk for injury.
YOU WANT UNBIASED ADVICE
Yoga instructors will want you to do yoga. Personal trainers will want you to come to their gym. Pilates instructors will want you to do Pilates. Strength coaches will want you to strength train. A physical therapist doesn’t have a bias or vested interest as to what type of fitness regimen you choose. They are only interested in helping you reach your goals.
YOU HAVE A HISTORY
If you have some kind of history that affects your ability to exercise, a PT is the best person to help you design a fitness regimen. It doesn’t matter if it’s an old injury from athletics or work, back pain that comes up from time to time, COPD, arthritis or heart disease, a PT can help you safely work around it and meet your fitness goals.
Want to Stay Healthy? Move More.
COVID has certainly made the importance of health very clear and we have all seen how quickly things can change with an illness. While COVID is currently front and center in most people’s thoughts, it isn’t the only thing out there that can change your life. Heart disease, diabetes, strokes and cancer can all be devastating too.
Movement Offers a Defense
If you’re looking to be more resilient and defend against these things, physical activity can do it. The dangers of being sedentary are well known and documented in the research. Excessive sitting and sedentary time have even been called the new smoking. For many of us, sitting and being inactive is part of our jobs. However, research has shown that getting in enough movement can counteract the negative effects of being sedentary.
A large study done in the U.K. found no association between the amount of time people spent sedentary and their chances of illness. But the authors didn’t conclude that being sedentary is OK. Instead, they felt their findings were likely “attributable to a protective effect of the high volumes of daily walking.” The study was conducted in London, where people tend to spend much more time walking or standing than average. The people in the study had daily walking times that were over double the average amount reported in the U.K.
Physical Therapists Are Unequaled Experts in Human Movement
While walking was the activity in this particular study, other research has shown that all kinds of movement can help protect your health. If you’re looking to get those protective benefits for yourself you could choose to walk, bike, lift weights, dance, or garden. If you’re not moving as much or as well as you’d like, see our physical therapists.
PTs are the most qualified professionals on the planet to help you move better and allow you to stay healthy and enjoy life. From designing a program to get you started or moving more to help you recover from an injury, your PT is the right person to look to for help!
