Pool (aquatic) exercise provides many benefits, including an ideal environment to exercise throughout the year. The buoyancy of the water supports a portion of your body weight making it easier to move in the water and improve your flexibility. The water also provides resistance to movements, which helps to strengthen muscles.
Pool exercises can also improve agility, balance, and cardiovascular fitness. Many types of conditions greatly benefit from pool exercise, including arthritis, fibromyalgia, back pain, joint replacements, neurological, and balance conditions. The pool environment also reduces the risk of falls when compared to exercise on land.
Preparing for the Pool
Before starting any pool exercise program, always check with your physical therapist or physician to make sure pool exercises are right for you. Physical therapists are movement experts who improve quality of life through hands on care, patient education, and prescribed movement.
Here are some tips to get you started:
- Water shoes will help to provide traction on the pool floor.
- Water level can be waist or chest high.
- Use a Styrofoam noodle or floatation belt/vest to keep you afloat in deeper water.
- Slower movements in the water will provide less resistance than faster movements.
- You can use webbed water gloves, Styrofoam weights, inflated balls, or kickboards for increased resistance.
- Never push your body through pain during any exercise.
- Although you will not notice that you sweat with pool exercises, it is still important to drink plenty of water.
10 Excellent Exercises for the Pool
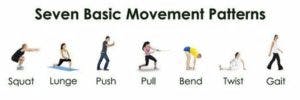
1. Water walking or jogging: Start with forward and backward walking in chest or waist-high water. Walk about 10-20 steps forward, and then walk backward. Increase speed to make it more difficult. Also, increase intensity by jogging gently in place. Alternate jogging for 30 seconds with walking in place for 30 seconds. Continue for 5 minutes.
2. Forward and side lunges: Standing near a pool wall for support, if necessary, take an oversized lunge step in a forward direction. Do not let the forward knee advance past the toes. Return to the starting position and repeat with the other leg. For a side lunge, face the pool wall and take an oversized step to the side. Keep toes facing forward. Repeat on the other side. Try 3 sets of 10 lunge steps. For variation, lunge walk in a forward or sideways direction instead of staying in place.
3. One leg balance: Stand on 1 leg while raising the other knee to hip level. Place a pool noodle under the raised leg, so the noodle forms a “U” with your foot in the center of the U. Hold as long as you can up to 30 seconds and switch legs. Try 1-2 sets of 5 on each leg.
4. Sidestepping Face the pool wall. Take sideways steps with your body and toes facing the wall. Take 10-20 steps in 1 direction and then return. Repeat twice in each direction.
5. Hip kickers at pool wall: Stand with the pool wall to one side of your body for support. Move 1 leg in a forward direction with the knee straight, like you are kicking. Return to start. Then move the same leg to the side, and return to the start position. Lastly, move that same leg behind you. Repeat 3 sets of 10 and switch the kicking leg.
6. Pool planks: Hold the noodle in front of you. Lean forward into a plank position. The noodle will be submerged under the water, and your elbows should be straight downward toward the pool floor. Your feet should still be on the pool floor. Hold as long as comfortable, 15-60 seconds depending on your core strength. Repeat 3-5 times.
7. Deep water bicycle: In deeper water, loop 1-2 noodles around the back of your body and rest your arms on top of the noodle for support in the water. Move your legs as if you are riding a bicycle. Continue for 3-5 minutes.
8. Arm raises: Using arm paddles or webbed gloves for added resistance, hold arms at your sides. Bend your elbows to 90 degrees. Raise and lower elbows and arms toward the water surface, while the elbows remain bent to 90 degrees. Repeat for 3 sets of 10.
9. Push-ups: While standing in the pool by the poolside, place arms shoulder-width apart on pool edge. Press weight through your hands and raise your body up and halfway out of the water, keeping elbows slightly bent. Hold 3 seconds and slowly lower back into pool. (Easier variation: Wall push up on side of pool: place hands on edge of pool shoulder-width apart, bend elbows, and lean chest toward the pool wall.)
10. Standing knee lift: Stand against the pool wall with both feet on the floor. Lift 1 knee up like you are marching in place. While the knee is lifted even with your hip, straighten your knee. Continue to bend and straighten your knee 10 times, and then repeat on the other leg. Complete 3 sets of 10 on each leg. For more of a challenge, try this exercise without standing against the pool wall.
—
source: https://www.choosept.com