Physical therapists aren’t just for people that are injured or have had surgery. Physical therapists can also help healthy people improve their fitness. Here are 5 reasons why you should consider seeing yours.
YOU WANT A BASELINE
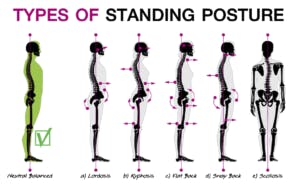
When you see a physical therapist to improve your fitness, you’ll get an assessment of your strength, range of motion, posture and movement patterns. This not only helps your physical therapist design a customized program just for you, it gives them a baseline to compare things to in the future should you start having pain or suffer an injury.
YOU WANT EXPERT GUIDANCE
Sure, other professionals could help with your fitness routine, but the fitness industry is not well regulated. Some certifications just require an online course and paying a fee. There are no licenses or other requirements to use many titles. Becoming a physical therapist requires at least a bachelor’s degree and most PTs practicing today have a doctorate. Every PT has passed a national board exam and maintains a state license. That guarantees you that every physical therapist is a verified expert in human movement.
YOU WANT TO PREVENT INJURY
Physical therapists don’t just work to heal injuries, they are also experts in preventing them. After a thorough assessment, a PT can help you design a program that will not only help you reach your fitness goals, but that can address any issues that increase your risk for injury.
YOU WANT UNBIASED ADVICE
Yoga instructors will want you to do yoga. Personal trainers will want you to come to their gym. Pilates instructors will want you to do Pilates. Strength coaches will want you to strength train. A physical therapist doesn’t have a bias or vested interest as to what type of fitness regimen you choose. They are only interested in helping you reach your goals.
YOU HAVE A HISTORY
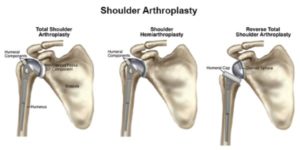
If you have some kind of history that affects your ability to exercise, a PT is the best person to help you design a fitness regimen. It doesn’t matter if it’s an old injury from athletics or work, back pain that comes up from time to time, COPD, arthritis or heart disease, a PT can help you safely work around it and meet your fitness goals.